How to Prevent Common Medical Claim Denials: A Guide for Medical Practices
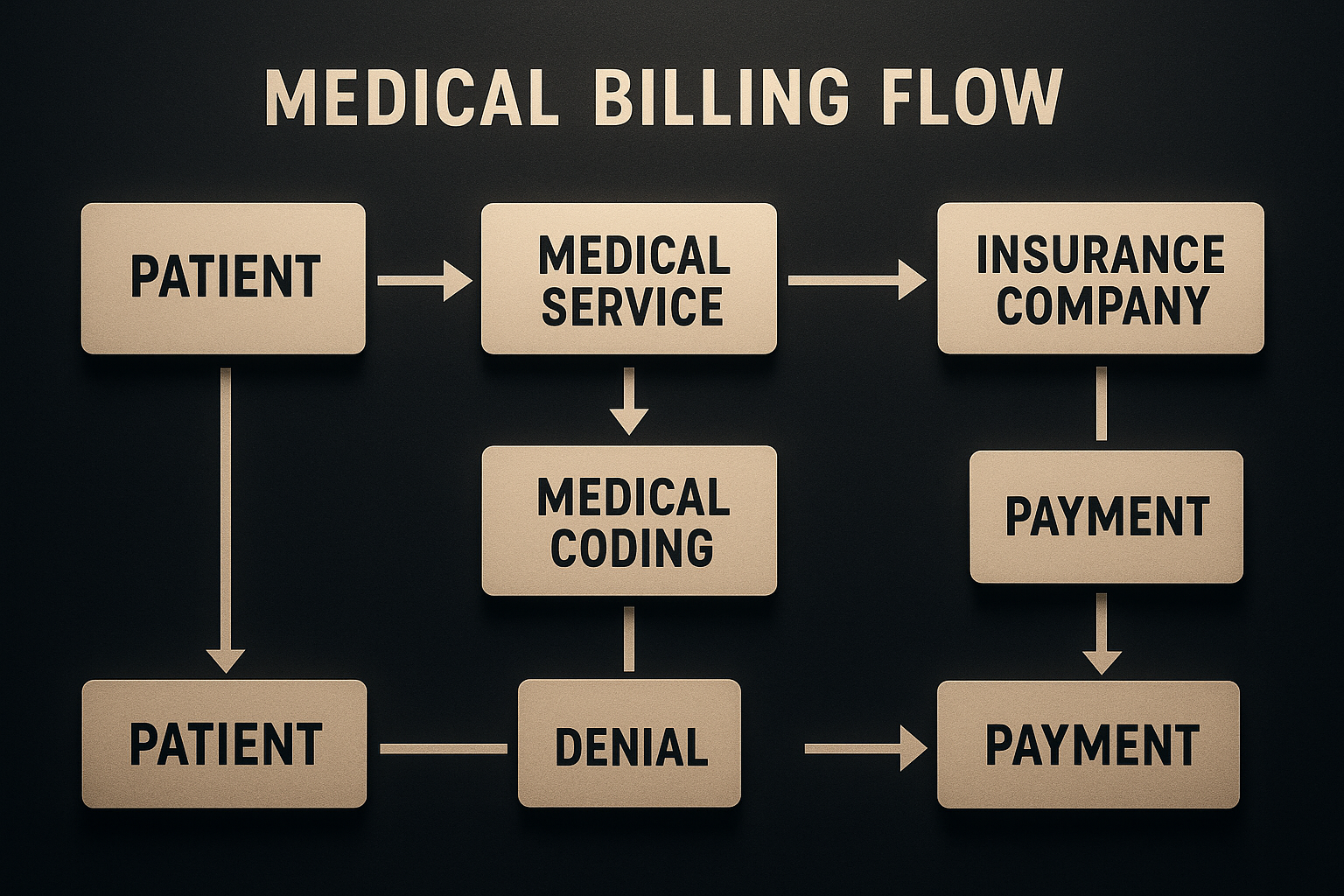
The financial health of any medical practice hinges on consistent revenue. Yet, medical claim denials can silently drain resources, disrupt cash flow, and burden your staff. Denials aren't minor issues; they directly impact your practice's ability to thrive.
This guide will reveal the common reasons claims are denied and, more importantly, provide practical steps to prevent medical claim denials, ensuring your practice's financial stability. Sometimes, expert support from a dedicated medical billing company like CHB can be the missing piece.
Understanding the Root Causes: Why Do Medical Claims Get Denied?
To prevent medical claim denials, you must first understand their origins. Denials rarely appear without cause; they typically stem from specific, often avoidable, errors within your revenue cycle. Up to 13% of all medical claims are denied on the first submission, highlighting a significant area for improvement. Let’s explore the most common medical claim denial reasons:
Inaccurate Patient Information/Demographics: Small errors like misspelled names, incorrect dates of birth, or transposed insurance IDs can lead to denials. Accurate data collection at the first point of contact is vital.
Missing or Wrong Insurance Details: Failure to secure pre-authorizations, referrals, or misunderstanding policy limitations often results in denials. Always verify eligibility and understand policy specifics before services are rendered.
Coding Errors (ICD-10, CPT, HCPCS): Incorrect or outdated codes for diagnoses, procedures, or supplies are frequent medical billing errors. Denials also occur due to insufficient medical necessity documentation, unbundling, or upcoding.
Lack of Medical Necessity Documentation: Insurance companies require clear justification for services. If clinical notes don’t fully support the diagnosis or treatment, claims will be denied. Thorough and specific clinical notes are crucial.
Timely Filing Limits Exceeded: Every payer enforces strict deadlines (typically 90-120 days) for claim submission. Submitting claims after this window, known as untimely filing, results in automatic, almost unappealable denials.
Duplicate Claims or Services: Submitting the same claim multiple times for the same service on the same day leads to denials. This often points to internal confusion or poor coordination.
Services Not in the Plan: While not always avoidable, services not covered by a patient’s insurance plan will be denied. Always communicate coverage limitations to patients.
How to Prevent Medical Claim Denials: Tips for Your Practice
Proactive strategies are essential for addressing medical claim denial reasons. These tips will not only reduce claim rejections but also strengthen your Revenue Cycle Management (RCM):
Step One: Supercharge Patient Verification
Verify insurance eligibility before each patient visit (policy status, copays, deductibles, specific coverage).
Collect updated demographic data every time, not just initially.
Utilize real-time eligibility checks via your practice management system.
Step Two: Master Medical Coding and Documentation
Provide regular training for coders and physicians on current ICD-10, CPT, and HCPCS guidelines.
Ensure comprehensive clinical documentation that fully supports every billed service and medical necessity.
Cross-reference services with diagnoses for logical consistency.
Step Three: Stick to Timely Filing Limits Like Glue
Establish clear workflows for immediate claim submission after services are rendered and documented.
Automate alerts in your billing software for claims approaching their filing deadlines.
Step Four: Boost Communication Among Your Team
Hold regular meetings to review denial trends and discuss common medical billing errors.
Implement a feedback system for billing staff to inform clinicians about documentation gaps and front office staff about verification issues.
Step Five: Embrace Technology: Invest in a Better RCM Software
Use automated scrubbing tools to identify and correct errors before claim submission.
Leverage real-time reporting and analytics to spot denial patterns quickly.
Ensure seamless integration between your billing software and Electronic Health Record (EHR) system.
Step Six: Regularly Audit Your Billing Processes
Conduct proactive internal audits of claim samples to identify weak spots and inefficiencies.
Use audit findings to continuously improve your systems and medical billing best practices.
The Benefits of Proactive Denial Management for Your Medical Practice
Successfully implementing strategies to prevent medical claim denials offers significant advantages:
Better Cash Flow and Stable Revenue: Leads to faster, more predictable income.
Reduced Administrative Costs and Happier Staff: Frees up staff from rework and appeals.
Stronger Compliance and Lower Audit Risk: Minimizes penalties and audit likelihood.
Smarter Financial Decisions: Accurate data empowers informed strategic choices.
Why Partnering with an Expert Medical Billing Company Like CHB Makes a Difference
While internal efforts are crucial, the complexity of medical billing often benefits from specialized outside expertise. Partnering with a dedicated medical billing company like CHB offers distinct advantages:
Specialized Expertise: CHB provides up-to-the-minute knowledge in complex medical billing, coding, and RCM.
Advanced Technology: We utilize cutting-edge RCM software to proactively identify and correct claim errors.
Dedicated Denial Management Teams: Our specialists excel at preventing and appealing denials to recover your revenue.
You Can Focus on Patients: Outsourcing billing allows your team to prioritize patient care.
Real Cost Savings: Our services can lower operational costs associated with billing, appeals, and lost revenue.
Conclusion
Preventing medical claim denials is paramount for a healthy medical practice. By understanding common denial reasons and implementing proactive strategies, your clinic can significantly reduce claim rejections, improve cash flow, and operate more efficiently.
While adopting these best practices in-house is beneficial, partnering with an expert medical billing company like CHB provides specialized knowledge and tools to truly enhance your revenue cycle management. Take control of your practice’s financial future by changing the way you handle medical claims.
How to Prevent Common Medical Claim Denials: A Guide for Medical Practices
як bangladesh country (2025-07-12)
З приводу Nutrition Education: How to Safely Use Psyllium Husk in Your Diet
How to Prevent Common Medical Claim Denials: A Guide for Medical PracticesThe financial health of any medical practice hinges on consistent revenue. Yet, medical claim denials can silently drain resources, disrupt cash flow, and burden your staff. Denials aren't minor issues; they directly impact your practice's ability to thrive.
This guide will reveal the common reasons claims are denied and, more importantly, provide practical steps to prevent medical claim denials, ensuring your practice's financial stability. Sometimes, expert support from a dedicated medical billing company like CHB can be the missing piece.
Understanding the Root Causes: Why Do Medical Claims Get Denied?To prevent medical claim denials, you must first understand their origins. Denials rarely appear without cause; they typically stem from specific, often avoidable, errors within your revenue cycle. Up to 13% of all medical claims are denied on the first submission, highlighting a significant area for improvement. Let’s explore the most common medical claim denial reasons:
Inaccurate Patient Information/Demographics: Small errors like misspelled names, incorrect dates of birth, or transposed insurance IDs can lead to denials. Accurate data collection at the first point of contact is vital.
Missing or Wrong Insurance Details: Failure to secure pre-authorizations, referrals, or misunderstanding policy limitations often results in denials. Always verify eligibility and understand policy specifics before services are rendered.
Coding Errors (ICD-10, CPT, HCPCS): Incorrect or outdated codes for diagnoses, procedures, or supplies are frequent medical billing errors. Denials also occur due to insufficient medical necessity documentation, unbundling, or upcoding.
Lack of Medical Necessity Documentation: Insurance companies require clear justification for services. If clinical notes don’t fully support the diagnosis or treatment, claims will be denied. Thorough and specific clinical notes are crucial.
Timely Filing Limits Exceeded: Every payer enforces strict deadlines (typically 90-120 days) for claim submission. Submitting claims after this window, known as untimely filing, results in automatic, almost unappealable denials.
Duplicate Claims or Services: Submitting the same claim multiple times for the same service on the same day leads to denials. This often points to internal confusion or poor coordination.
Services Not in the Plan: While not always avoidable, services not covered by a patient’s insurance plan will be denied. Always communicate coverage limitations to patients.
How to Prevent Medical Claim Denials: Tips for Your PracticeProactive strategies are essential for addressing medical claim denial reasons. These tips will not only reduce claim rejections but also strengthen your Revenue Cycle Management (RCM):
The Benefits of Proactive Denial Management for Your Medical PracticeStep One: Supercharge Patient Verification
Verify insurance eligibility before each patient visit (policy status, copays, deductibles, specific coverage).
Collect updated demographic data every time, not just initially.
Utilize real-time eligibility checks via your practice management system.
Step Two: Master Medical Coding and Documentation
Provide regular training for coders and physicians on current ICD-10, CPT, and HCPCS guidelines.
Ensure comprehensive clinical documentation that fully supports every billed service and medical necessity.
Cross-reference services with diagnoses for logical consistency.
Step Three: Stick to Timely Filing Limits Like Glue
Establish clear workflows for immediate claim submission after services are rendered and documented.
Automate alerts in your billing software for claims approaching their filing deadlines.
Step Four: Boost Communication Among Your Team
Hold regular meetings to review denial trends and discuss common medical billing errors.
Implement a feedback system for billing staff to inform clinicians about documentation gaps and front office staff about verification issues.
Step Five: Embrace Technology: Invest in a Better RCM Software
Use automated scrubbing tools to identify and correct errors before claim submission.
Leverage real-time reporting and analytics to spot denial patterns quickly.
Ensure seamless integration between your billing software and Electronic Health Record (EHR) system.
Step Six: Regularly Audit Your Billing Processes
Conduct proactive internal audits of claim samples to identify weak spots and inefficiencies.
Use audit findings to continuously improve your systems and medical billing best practices.
Successfully implementing strategies to prevent medical claim denials offers significant advantages:
Better Cash Flow and Stable Revenue: Leads to faster, more predictable income.
Reduced Administrative Costs and Happier Staff: Frees up staff from rework and appeals.
Enhanced Patient Satisfaction: Fewer billing surprises improve patient experience.
Stronger Compliance and Lower Audit Risk: Minimizes penalties and audit likelihood.
Smarter Financial Decisions: Accurate data empowers informed strategic choices.

Why Partnering with an Expert Medical Billing Company Like CHB Makes a DifferenceWhile internal efforts are crucial, the complexity of medical billing often benefits from specialized outside expertise. Partnering with a dedicated medical billing company like CHB offers distinct advantages:
ConclusionSpecialized Expertise: CHB provides up-to-the-minute knowledge in complex medical billing, coding, and RCM.
Advanced Technology: We utilize cutting-edge RCM software to proactively identify and correct claim errors.
Dedicated Denial Management Teams: Our specialists excel at preventing and appealing denials to recover your revenue.
You Can Focus on Patients: Outsourcing billing allows your team to prioritize patient care.
Real Cost Savings: Our services can lower operational costs associated with billing, appeals, and lost revenue.
Preventing medical claim denials is paramount for a healthy medical practice. By understanding common denial reasons and implementing proactive strategies, your clinic can significantly reduce claim rejections, improve cash flow, and operate more efficiently.
While adopting these best practices in-house is beneficial, partnering with an expert medical billing company like CHB provides specialized knowledge and tools to truly enhance your revenue cycle management. Take control of your practice’s financial future by changing the way you handle medical claims.